‘Today is day 93’: People report experiencing COVID-19 symptoms that last for months
LOS ANGELES - Since the first reported cases of the novel coronavirus, several support groups have emerged on Facebook consisting of thousands of members calling themselves “long haul survivors,” reporting COVID-19 symptoms that they say have lasted for months.
“Today is day 93,” said Amy Watson, a preschool teacher who lives in Portland, Oregon as she shared a photograph of her thermometer that read 100.3 on June 18. She first tested positive for COVID-19 on April 11, after falling ill with flu-like symptoms in mid-March.
Watson said she has had a persistent fever for nearly three months now, along with a handful of other disconcerting symptoms.
RELATED: CoronavirusNOW.com, FOX launches national hub for COVID-19 news and updates

Photograph of Amy Watson’s temperature taken on June 18. (Credit: Amy Watson)
Watson said she first came down with the flu-like symptoms on March 15, when she developed a cough and fever. She felt some of the worst of the illness for about a week, until, she said, she started to feel better, only to have the illness return like “a ton of bricks.”
While she said the initial symptoms of congestion and cough have since subsided, she continues to experience other manifestations of the illness.
“These other symptoms that have just been hanging on are the ones that nobody knows how to treat and fix,” said Watson. “I’ve got this fever, I got this crazy burning sensation, nerve pain that’s like under my skin, incredible fatigue.”
Watson, whose only underlying condition before contracting COVID-19 was asthma, added that she has to sit down and rest every time she performs any menial task.
Back in March when she first reported feeling sick, it was nearly impossible for her to get a COVID-19 test. She said she called an advice nurse, who told her to assume it was the novel coronavirus and isolate herself for two weeks, which she did.
“The 14 days passed and I was still sick,” said Watson. She was prescribed multiple rounds of antibiotics after she reached three weeks of being symptomatic with the illness.
RELATED: Dr. Fauci says 'it will be when not if' for a COVID-19 vaccine
The problem with testing
Watson’s long-term fever sparked concerns that she might have cancer, but after several lab tests, her results came back “normal.” At that point, Watson said she was told that only medical workers and front-line responders to the coronavirus were permitted to take a COVID-19 test in her area.
But because of her asthma, she was finally able to get tested, nearly a month into her illness. Two days later, the test came back positive.
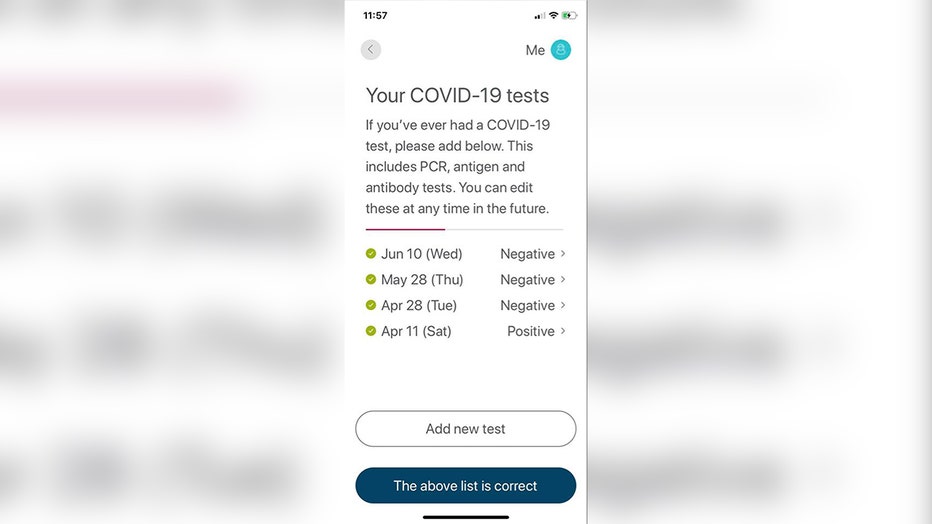
A screenshot of Amy Watson’s COVID-19 test results.
Despite Watson testing negative for the novel coronavirus at the end of April, she still felt sick, and doctors gave her the discouraging news that she should expect at least another eight weeks before fully recovering from the disease.
Watson’s experience with testing also resonated with many members of the various “long haul” Facebook groups. Many said they have simply been unable to get tested.
Health officials have said that testing in the United States early on was insufficient for optimal containment of the virus. In early March, Dr. Anthony Fauci, a member of the White House coronavirus task force, testified that the nation's testing system was “not really geared to what we need right now” and added, “it is a failing. Let’s admit it.”
By mid-February, when some of the first CDC coronavirus tests were administered, technicians reported getting inconclusive results, which the CDC said could be due to the test looking for signs of generic coronaviruses, of which there are many, rather than the specific virus that causes COVID-19.
By then, only about a half-dozen state and local public health labs had reliable tests.
In March, President Donald Trump assured Americans that the COVID-19 test developed by the Centers for Disease Control and Prevention was “perfect” and that “anyone who wants a test can get a test.” But more than two months after the first U.S. case of the new disease was confirmed, many people still could not get tested.
When Watson was still experiencing symptoms long after testing negative for the virus, she decided to search for others with a similar experience. She found several COVID-19 support groups on Facebook, many of which she said consisted of members who did not actually suffer from the virus.
Watson said she had a negative experience with people in those groups, so she decided to start her own after connecting with other people who she said “sounded like me.”
She said she initially expected the group to have maybe a dozen members when it started on April 29, but it has since drawn more than 3,000 people from over 58 countries.
“The group has been an amazing source of comfort,” said Watson. “On our header it says, ‘welcome, no you’re not crazy and you’re not alone.’”
Since the group’s creation, Watson and other members have started a petition, which had received 9,367 signatures as of June 22, in hopes of clarifying official COVID-19 guidelines to “accurately reflect recovery periods.”
Currently, the U.S. Centers for Disease Control and Prevention recommends that individuals who contract the novel coronavirus self-isolate for 14 days. A report from the World Health Organization said that “the median time from onset to clinical recovery for mild cases is approximately 2 weeks and is 3-6 weeks for patients with severe or critical disease.”
In an interview regarding recent increases in coronavirus cases in the U.S., Dr. Tom Tsai, a surgeon and health policy researcher at Harvard T.H. Chan School of Public Health, said he had not heard of stories like Amy’s, most likely because “we are still in the midst of it.”
“I don’t think we have enough clinical or medical data,” said Tsai. “I haven’t seen anything in the medical literature about the long-term consequences from COVID infections, and that is probably just because it’s only been six months since COVID reared its head.”
Tsai added that while most disease models suggest that people recover from the virus from a transmissibility standpoint, there is not enough information to understand the long-term effects of the novel coronavirus in terms of symptoms, calling instances like Watson’s and other “long haul survivors,” a “legitimate concern.”
“It’s important to study that [long-term effects of COVID-19], the hard part is that COVID symptoms are so vague, and it’s so variable,” said Tsai. “People dying, people in the ICU, people who have almost no symptoms, that’s part of the challenge of the pandemic is that its effect is so variable across populations, across different demographic groups, different ages.”
“I think it’s too early to know whether this is truly people who may be at risk for a longer disease course,” Tsai said.
RELATED: The battle is not over: Rising coronavirus infections seen worldwide
‘COVID toes’ and other anomalous effects of the virus
Dr. Mady Hornig, an immunologist and professor of epidemiology at Columbia University who is currently researching the long-term effects of a viral infection like COVID-19, has been confronted with an array of concerning symptoms that have persisted in patients, as well as herself.
Hornig can personally attest to the variety of symptoms that have been reported in coronavirus patients, ever since she began to experience COVID-19 symptoms herself in April that have continued to impact her daily life for the past 11 weeks.
Hornig listed an array of long-term effects that she and her fellow researchers are finding in COVID-19 patients, including one illness that has been frequently described in the “long haul” Facebook groups, and by Watson as well. It has been referred to as “COVID toes.”
Hornig said she’s not entirely clear on what can cause such a symptom, but said that she did experience swelling in her feet.
When sufferers describe “COVID toes,” they describe a painful swelling in their feet in which red or purple lesions can develop on fingers or toes.
The most common coronavirus symptoms are fever, a dry cough and shortness of breath -- and some people are contagious despite never experiencing symptoms. But as this bewildering virus continues to spread, less common symptoms are being reported including loss of smell, vomiting and diarrhea, and increasingly, a variety of skin problems.
In one report, dermatologists evaluated 88 COVID-19 patients in an Italian hospital and found 1 in 5 had some sort of skin symptom, mostly red rashes over the trunk. In another, Spanish doctors reported a series of 375 confirmed virus patients with a range of skin complaints, from hives to chickenpox-like lesions to the toe swellings.
Pictures of reddened toes and rashes all over social media and doctor chat groups have “already enabled the rapid recognition of skin signs by dermatologists. It is now time for rigorous science” to understand the link, Dr. Kanade Shinkai of the University of California, San Francisco wrote in a recent JAMA Dermatology editorial.
Since getting sick, Hornig said she’s had to carry a pulse oximeter with her, a device which registers her pulse since she began to have tachycardia episodes when her fever began to decline. Tachycardia is a condition that can make your heart beat abnormally fast, reducing blood flow to the rest of your body, according to The Mayo Clinic.
Her most recent episode was on June 22. Her pulse registered at 135 beats per minute, which she said occurred just from her sitting at her computer. She said a normal pulse for someone her age would be around 60-70 beats per minute.
Watson also said that her heart rate has been known to escalate and drop dramatically since she has been sick, and she said she was forced to go to urgent care after an incident she had last week when she thought she was having a heart attack.
While it was not a heart attack Watson was experiencing, she was diagnosed with pleurisy, a very painful illness in which tissue that separate the lungs from the chest wall becomes inflamed.
While symptoms like “COVID toes” and month-long fevers have left some medical workers perplexed, some illnesses stemming from the coronavirus are not entirely without precedent.
Hornig has been researching one particular illness that has previously been linked to other coronaviruses like SARS and MERS.
According to the CDC, coronaviruses are a large family of viruses that are common in people and many different species of animals. Many people have previously experienced a coronavirus in the form of the common cold. But COVID-19 has not previously been identified in humans
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is an illness Hornig said has been found in patients who have recovered from coronaviruses such as SARS. The CDC cites a 2015 report from the nation’s top medical advisory body, the Institute of Medicine, which says that an estimated 836,000 to 2.5 million Americans suffer from ME/CFS.
The CDC says that people with ME/CFS experience severe fatigue, sleep problems, as well as difficulty with thinking and concentrating while experiencing pain and dizziness.
Hornig said SARS-CoV-1 and MERS have been associated with longer-term difficulties, in which many people appeared to have symptoms of ME/CFS.
In April, advocates of the Solve ME/CFS Initiative (Solve M.E.) virtually stormed Capitol Hill for the fourth annual ME/CFS Advocacy day, which the organization calls a “national event to educate congress about the neuroimmune disease.”
According to the organization, "Some COVID-19 patients are exhibiting Me/CFS-like symptoms (nearly 35% of patients)" adding that the illness typically follows a viral infection.
“ME/CFS is an urgent public health crisis based on what is happening in our country right now,” says Emily Taylor, Director of Advocacy and Community Relations at Solve M.E. “Evidence suggests that a virus as serious and widespread as COVID-19 could ignite rapid and significant growth in the ME/CFS population in just 36 months This is a very real, science-based concern, adding an even stronger sense of urgency to take action today. We must get the attention of our country’s leaders.”
Despite ‘long haul’ sufferers, pandemic still in early stages
After personally experiencing her own mysterious and frustrating long-term COVID-19 effects, Hornig reiterated the importance of studying cases like Watson’s as an opportunity to learn the potential future effects of a viral infection like the novel coronavirus.
“We owe it to these patients to really take these issues seriously,” Hornig said. “It’s a challenge because we may have missed the window for getting the right diagnosis, people may no longer be infectious, and we don’t know how long the antibodies are going to last.”
And while the term “long haul” has been coined for people who have experienced COVID-19 symptoms for months now, medical experts like Hornig are emphasizing that much is still unknown about the disease and that we still may be in an early stage of the pandemic.
Alarming surges in coronavirus cases across the U.S. South and West raised new fears Monday that the outbreak is spiraling out of control and that hard-won progress against the scourge is slipping away because of resistance among many Americans to wearing masks and keeping their distance from others.
Confirming predictions that the easing of state lockdowns over the past month-and-a-half would lead to a comeback of the virus, cases surpassed 100,000 in Florida, hospitalizations are rising dramatically in Houston and Georgia, and a startling 1 in 5 of those tested in Arizona are proving to be infected.
Over the weekend, the virus seemed to be everywhere at once: Several campaign staff members who helped set up President Donald Trump's rally in Tulsa, Oklahoma, tested positive, as did 23 Clemson University football players in South Carolina. At least 30 members of the Louisiana State University team were isolated after becoming infected or coming into contact with someone who was. Meatpacking plants were also hit with new outbreaks.
“It is snowballing. We will most certainly see more people die as a result of this spike,” said Dr. Marc Boom, CEO and president of Houston Methodist Hospital, noting that the number of COVID-19 hospital admissions has tripled since Memorial Day to more than 1,400 across eight hospital systems in the Houston metropolitan area.
He warned that hospitals could be overwhelmed in three weeks, and he pleaded with people to cover their faces and practice social distancing.
“It is possible to open up at a judicious pace and coexist with the virus, but it requires millions and millions of people to do the right thing," Boom said.
Texas is among a number of states — including Arizona, Alabama, Florida and South Carolina — whose governors have resisted statewide mask requirements, leaving the matter to local authorities.
The number of new coronavirus cases across the country per day has reached more than 26,000, up from about 21,000 two weeks ago, according to an Associated Press analysis of data compiled by Johns Hopkins University. Over 120,000 deaths in the U.S. have been blamed on the virus, the highest toll in the world.
The Associated Press contributed to this story.





